A lot of my social media recently has been based around pain, pain science, the mechanisms of pain (chronic pain, particularly), and how pain can develop. It’s a tricky area at the best of times, and trying to translate the deep scientific reasoning is incredibly hard. But having spoken to a few of my peers over these recent posts, I – and I really mean we – still have such a long way to go in communicating the importance of this understanding.
The crux, really, to me is; We – therapists – are not mechanic’s.
You, patients, are not machines.
Not every presentation in clinic is purely mechanical. Sure, there will often be a physical process and involvement in the onset of pain (think running injury, shoulder pain, lower back pain or any acute condition), but handing out the same standard treatment to everyone who presents in pain, regardless of their condition, history, or aims has to stop.
It is a tale as old as time;
Step 1: Carry out tests that will “find” nothing more than completely normal individual variances (think “one leg longer than the other”, “twisted pelvis”, “wear and tear”) and then highlight these as the definite cause. Provide no evidence of causality at this stage.
Step 2: Crack the mid back, crack the neck, crack the lower back – regardless of where the pain has presented. The knee bone is connected to the thigh bone, afterall.
Step 3: DO NOT retest to show how this mechanical dysfunction has now been resolved. This is especially important if you have taken an X-ray prior to treatment.
Step 4: Book in for next week for more of the same.
10 minutes on the Therapists couch, for at least 12 weeks (until the “maintenance” sessions kick in, usually monthly), and a wallet at least £40/£60 lighter every time.
Pain is a unique, individual and personal experience, and a key component of managing, or removing that pain is understanding the condition.
I am a manual therapist (soft tissue, joint mobilisation, joint articulation etc) by trade, and we know that manual therapies can and do help – and sometimes we don’t even know why they help – but they do (1)! So we should use them. Our job is to help you have less pain! I do have my own thoughts and theories on how these work, and I am happy to discuss these with the person in pain at all times. But I do not claim to be aligning spines and pelvis’ with my bear hands, or readjusting the length of your legs – see footnote at the bottom*
But if you leave an appointment without the knowledge of why you are in pain, or without confidence in what you can do to help yourself, then you can become reliant on the therapy and/or therapist, rather than yourself. And I believe this to be bad for not just your recovery from pain, but also both your mental health well-being, and your wallet.
We (Therapists) have to be brave enough to think harder about why pain is present – we shouldn’t hide behind the skills we have, because we feel vulnerable away from them. See Cognitive Dissonance.
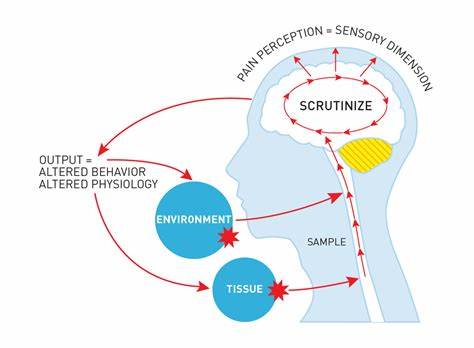
When you (the Patient) feel your pain (or do not feel your pain), and the circumstances thereof, can be as telling as where anatomically you feel your pain. We should consider the Bio-Psycho-Social Model of pain, whereby there are of course (as touched upon) BIOlogical aspects to consider, such as physical health, tissue health, and genetic variance. But there are also PSYCHological considerations, such as mental-health wellbeing, your own personal belief systems and stress levels. Throw into the melting pot the SOCIAL part, which includes relationships with your peers (and potential pressures, or even over concern from) friends, work colleagues and family members, and often the middle of this Venn Diagram of your control centre is………PAIN
If we address only one of these (often the BIO, because of social norms, acceptance and expectation – not to be dismissed, of course, but not to be preyed upon either) particularly with those of you suffering with chronic, long-standing pain, we are potentially missing huge parts of your story.
This is similar to what Louis Gifford termed the Mature Organism Model – see image below
So how can I help?
I do not specialise in any particular injury type, approach, treatment or philosophy. I use a lot of pre-prepared visuals and documents to support and describe our chosen treatment plan, and why we are taking that path, so you can have confidence that we are utilising all of the most current and relevant approaches, and not simply the ones that “sell” or rely on multiple visits.I believe that we all have a ‘Pain-on’ and a ‘Pain-off’ setting, and that at the root of this is an understanding of *why* you are in pain.
I believe that when you understand this, you start to regain that control.
What you will not get is never-ending treatment plans, which consist of only hands-on therapy, giving control to – and so building reliance on – the therapist (me!).
I do not want to see you every 4 weeks (lovely as you are ![]() )
)
I will never tell you you are broken, or that you need an MOT.
I will never suggest “at least X” number of sessions.
Message me if you would like to know more ![]()
1. ![]() Effectiveness of treatments for acute and subacute mechanical non-specific low back pain: a systematic review with network meta-analysis. Gianloa et al., (2021)
Effectiveness of treatments for acute and subacute mechanical non-specific low back pain: a systematic review with network meta-analysis. Gianloa et al., (2021)
*’Hyperstimulation analgesia’ is the partial (or sometimes total) relief of pain produced by a form of intense sensory stimulation. This sensory stimulation can be, well, almost anything – physical or otherwise. And that can – and often does – include a pain experience somewhere else. I have a lady I am working with currently who I saw 5 days pre-Total Knee Replacement (TKR), for an incredibly sore shoulder which she had been unable to use at all for over 10 days. I saw the same lady 10 days post TKR and asked about her shoulder – she had been completely unaware of any shoulder pain since the operation.
What a therapist I must be! Or…
The dorsal horn of the spinal cord primarily acts as the termination of primary afferent – incoming sensory – fibers. This modulation can be “bottom up” (i.e. from tissue, such as muscle), or “top down” (i.e. from the brain). This modulation is hugely influenced by what is going on elsewhere in the environment – in the body, within the nervous system, and within the mind of the individual. So, pain elsewhere (or mood, or tiredness, or stress or almost any intense sensory change) will have an effect on pain. Pain can kill pain!
So one to ponder going forwards:
What do you think that deeeeeeeep and painful sports massage, or that almighty clunk of your spine, or those sharp needles – or even prolonged ice/cryotherapy – may have done?
Helped? Undoubtedly.
In the way that you may have thought/been told? Perhaps not…
FURTHER READING: Aches & Pains, L. Gifford, Section 5: The Dorsal Horn.